Abstract
FLT3-ITD mutations are among the most common somatic mutations in acute myeloid leukemia (AML) and are important in prognostic determination as well as therapeutic allocation. Recent studies have demonstrated improved outcomes with the addition of FLT3 inhibitors and for some patients hematopoietic stem cell transplant (HSCT) in first remission (CR1). We have previously demonstrated that the outcome of FLT3-ITD patients can be quite heterogeneous based on the co-occurrence of a few specific risk stratifying mutations, including NPM1 and NUP98-NSD1. We sought to interrogate the complex landscape of cooperating events with FLT3-ITD AML and potential impacts on outcome in the context of contemporary therapies, including the FLT3 inhibitor sorafenib.
Of the 1296 children and young adult patients with de novo AML enrolled on COG AAML1031, 229 had FLT3-ITD mutations and were included in this study. Patients with high allelic ratio (HAR; >0.4) FLT3-ITD were allocated to Arm C, received sorafenib in combination with chemotherapy and received HSCT in CR1. Those with low allelic ratio (LAR; £ 0.4) FLT3-ITD were treated on Arm A/B and received chemotherapy, no sorafenib, and did not receive HSCT in CR1 unless they had evidence of residual disease following induction I (MRD³ 0.1%) or a high-risk cytogenetic feature. FLT3-ITD status and allelic ratio were determined by PCR and all samples also underwent karyotyping, FISH, and next generation sequencing in 195 (85%) of cases for determination of comprehensive co-occurring mutational profile.
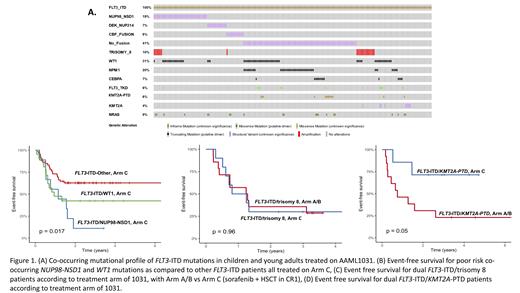
Among the 229 FLT3-ITD positive patients, allelic ratio ranged from <0.1-20.8, with 96 (42%) patients classified as LAR and 133 (58%) patients as HAR. Among the cohort overall, the significant majority of 85% (n=195) harbored a cooperating genomic aberration. The most common co-occurring single gene mutations were: WT1 (31%, n=71), NPM1 (20%, n=46), NRAS (9.2%, n=21), FLT3-TKD (7%, n=16), CEBPA (6.5%, n=15), KMT2A-PTD (5.7%, n=13) (Figure 1A). KMT2A-PTD lesions were significantly more prevalent among FLT3-ITD vs non ITD patients, 5.7% vs. 0.65% (p<0.001). Normal karyotype was detected in 50% of patients. The most common recurring cytogenetic abnormalities were NUP98-NSD1/t(5;11) fusions (19.2%, n=44), trisomy 8 (10%, n=23), DEK-NUP214/t(6;9) fusions (7%, n=16), KMT2A rearrangements (3.9%, n=9)(Figure 1A). In contrast, the other high risk abnormalities (monosomy 5/del5q, monosomy 7) were absent or exceedingly rare, while the low risk lesions t(8;21) and inv(16) were also rare (3%, n=7 each). We have previously reported outcome of the more common and risk stratifying mutations with co-occurring NUP98-NSD1 resulting in dismal prognosis regardless of treatment arm, while outcome for those with WT1 was improved with Arm C treatment and approached that of other FLT3-ITD patients(Figure 1B). Evaluation of the FLT3-ITD/trisomy 8 patients demonstrated those treated on Arm C experienced poor outcomes with an EFS of 30% and was equivalent to 29% for those on Arm A/B (p=0.96, Figure 1C), with a corresponding OS of 40% vs. 34% (p=0.66) respectively. In contrast, evaluation of outcome of the KMT2A-PTD patients demonstrated those treated on Arm C had a favorable 5-year event-free survival (EFS) of 71% vs. 23% (p=0.05) for those on Arm A/B (Figure 1D), with a corresponding 5-year overall survival (OS) of 86% vs. 46% (p=0.15) respectively.
Comprehensive sequencing demonstrated the FLT3-ITD samples identified co-occurring genetic mutations or cytogenetic abnormalities in the majority of cases. Although KMT2A-PTD is rarely reported in pediatric compared to adult AML, we found it was enriched in FLT3-ITD patients and this cohort experienced favorable outcomes when treated with transplant and sorafenib. Patients with dual FLT3-ITD/trisomy 8 had suboptimal outcomes similar to other poor risk co-occurring lesions and comparable regardless of AR or treatment arm. While there was some overlap with WT1 mutations in this cohort, further investigation into prognostic impact of this cooperating event is warranted. The prognostic implications FLT3-ITD mutations vary and we provide further data that the comprehensive cooperating mutational profile is critical to understanding the prognostic implications in specific patients, and may also impact response to FLT3 inhibitor therapy.
Hylkema: Moderna: Current equity holder in publicly-traded company; Quest Diagnostics Inc: Current equity holder in publicly-traded company. Pollard: Kura Oncology: Membership on an entity's Board of Directors or advisory committees; Syndax: Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal